Stroke, cancer and heart disease pose the biggest challenges for medicine in the developed world. But advances in tissue engineering and nanotechnology, combined with a better understanding of personal genetic factors, mean that successful treatments for these degenerative conditions could be just around the corner.
Where do medical advances come from? The obvious answer is that they are a product of the knowledge, observational skills and imagination of individual physicians and surgeons – but that is rarely the full story.
Traditionally, most developments in medicine are borne out of discoveries in basic biology. That may be new findings by physiologists or cell biologists about the way the human body works. Or it may be the identification by botanists and pharmacologists of new drugs that will modify those functions.
Yet, in this era of rapid medical progress, there is a new factor at work – collaborations between medics and experts from the physical sciences. Research in physics, materials science, computer technology and engineering is driving each of the three branches of medicine that show most promise for improving human health: personalised medicine, tissue engineering and nanotechnology.
Interdisciplinary research is the buzzword used in university medical faculties throughout the developed world. The underlying reason for this is that doctors have already picked the low-hanging fruit of easily treated diseases – straightforward interactions between humans and a disease pathogen or simple defects in a particular organ.
What remains to be fixed are conditions affecting complex body systems, like the immune response or the human brain, the most intricate object known. Often the problem is an interaction between genetics and the environment over time that produces the degenerative conditions – cancer, stroke and heart disease – which are the main cause of death in wealthy societies. Progress in understanding these diseases is only possible through the tools developed by physical sciences research, such as advanced imaging technologies and the computers that enable rapid analysis of huge quantities of data.
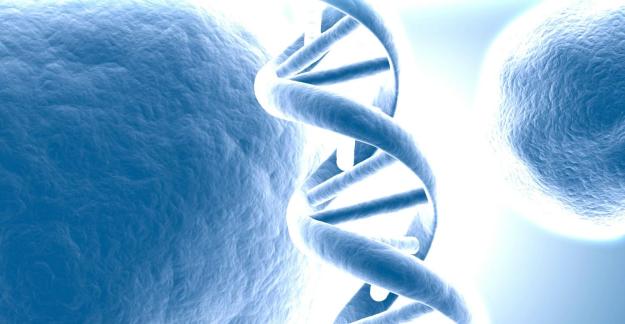
Personalised medicine – treatments specifically designed to take account of an individual’s genetic make-up – has become a possibility through the advances in mechanised gene sequencing technologies that have cut the time and cost involved in analysing human DNA. When the first draft of a representative human genome was announced in 2000, the researchers involved had spent around $3 billion during ten years of effort. Eight years later, the genome of James Watson (who 55 years earlier discovered the structure of DNA with Francis Crick) was completed in only a few months at a cost of $1 million. Then, in 2010, the gene defect responsible for the neurological condition Charcot-Marie-Tooth syndrome was identified in the DNA of James Lupski, another genomics pioneer. That was the first time gene sequencing had been used to find the cause of a disease in an individual and the project cost only $50,000. As an editorial in the New England Journal of Medicine observed, “The cost is fast approaching the threshold at which DNA sequencing will become a routine part of the diagnostic armamentarium”.
Identifying mutations that cause rare genetic diseases is only one aspect of personalised medicine. More importantly, it will also help detect those factors that may make some individuals more vulnerable to multifactorial conditions like heart disease. That will shift the emphasis in medicine from treatment to prevention by allowing people to adjust their diet and lifestyle to reduce the risk.
It will also help to ensure that any treatments that are given to patients will work. Genetic factors can strongly influence our response to particular medical treatments. So, for example, only about one in four women with breast cancer will benefit from the monoclonal antibody-based drug Herceptin, which targets a particular protein on the cell surface of some tumour cells. As a result, patients are now tested to see if they will react positively to an expensive drug that is highly effective in the right person, and useless in others. Already about 10 percent of the new drugs being licensed by the US government’s Food and Drug Administration are sold with information about which groups of the population they are intended for – that figure is sure to increase considerably over the next decade.
Tissue engineering is another rapidly growing branch of medical science devoted to rebuilding body parts that have been lost or damaged by disease, accident or everyday ‘wear and tear’. In most cases, it is dependent on stem cell technology, using the undifferentiated cells found in nearly all tissues that are capable of developing into any one of the hundreds of different cell types found in the body.
Stem cells have been extracted from human embryos, umbilical cords and even the fat tissue removed during cosmetic liposuction procedures. However, the eventual goal will be to collect stem cells from the patient’s own body and grow them in tissue culture until there is enough to be useful in a major medical procedure. That way they can be implanted back in the patient’s body without him or her having to take drugs to suppress the immune system and prevent rejection, as may occur with tissue from unrelated donors.
The major challenges in this branch of science (also known as regenerative medicine) are in achieving precise control over how the cells develop and in encouraging them to adopt an appropriate three-dimensional shape. Without the biological forces that guide such development in the body, stem cells will either grow to form a shapeless blob or a thin sheet of cells. The latter option has proved satisfactory when creating some relatively simple bodily structures such as a new windpipe, artificial skin, bladder and corneas. But it may be some time before more complex three-dimensional structures like joints become available for human patients (see box), let alone whole organs like a heart or liver.
Nanotechnology is the use of microscopic structures between 1 billionth and 100 billionth of a metre in size to create new diagnostic or therapeutic products. Although it is being billed as a new frontier in medicine, nanotechnology-based agents have been available for at least 15 years and there are more than 40 examples already on the market. In the first of these, the cancer drug doxorubicin was encapsulated in minute lipid spheres, called liposomes, so that it could be injected into the body and reach its destination in the tumour cells without being destroyed by the body’s immune system.
Another form of nanotechnology currently being tested in a range of medical applications is the use of hollow carbon or metal tubes as packaging for drug agents or as contrast agents to improve the clarity of the images produced by imaging scanners. One promising experimental application involves using gold particles linked to monoclonal antibodies that direct the combination to a tumour. After receiving the drug, that part of the patient’s body is irradiated with a laser and the energy is absorbed by the gold particles, which then heat up and cook the surrounding cancer cells.
However, when applying a powerful but largely unproven technology for the fi rst time, there is always the risk of producing unexpected results. So the pace of change in medicine, as a result of new disciplines like nanotechnology, may be determined as much by the need to prove their safety as by the rate of advances in the underlying science. Whoever is now driving the juggernaut of medical progress – the physician, surgeon or even the mechanical engineer – they will always need to obey the maxim that medical students have been taught since ancient times: Primum non nocere – first, do no harm.